You might have seen that a group of scientists recently shared news of a highly virulent strain of HIV (here’s their work in full). But what does this mean for HIV prevention and people living with HIV? The short answer is: not very much. This strain still seems to respond to treatment, so it can still be controlled, and PrEP can still prevent it. Also this strain isn’t actually new, it’s been around for years, the new research just looks at how it has spread between people in the Netherlands. But I still wondered what we know about HIV types?
Welcome to the HIV zoo
I haven’t spent a lot of time studying HIV, so I went to see what I could find out. AVERT, a charity that aims to improve understanding of HIV and sexual health, have a fantastic section about different types of HIV (which you should read for more details).
HIV is a virus which means, just like us, it has genes. Viruses cause infections by making thousands of copies of themselves that invade healthy cells and each time viruses copy themselves they have to copy their genes too. Copying genes is like writing out a coded message, for HIV the message is about 9,000 letters long. If you do it thousands of times you’re going to make mistakes and that’s how viruses change.
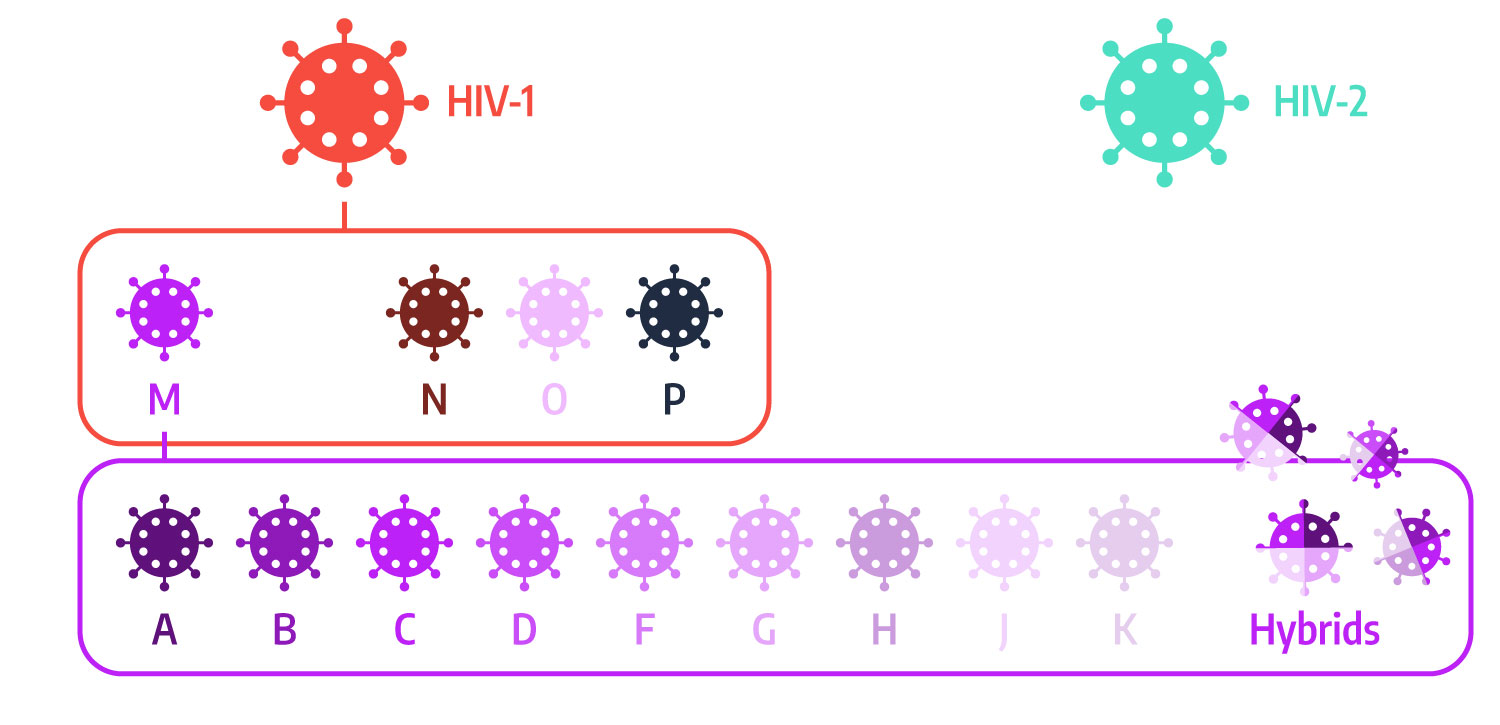
So where is HIV at? Well, HIV changes a lot and it happens so much that we don’t even name all the different forms. We do have some names though (check out the image below): First, there are two main types of HIV virus, HIV-1 and HIV-2. Almost all cases of HIV are caused by HIV-1. Only about 1 in 20 HIV cases are caused by HIV-2 and these are mostly linked to West Africa. HIV-2 is harder to spread and progresses more slowly than HIV-1 but we know a lot less about treating it effectively.
There are four types of HIV-1, called groups M, N, O and P. Most cases are caused by group M but, again, the other groups are more common in certain places, largely parts of Africa.
But wait, there’s still more. HIV-1 group M has at least nine subtypes, helpfully called A, B, C, D, F, G, H, J and K (Don’t ask what happened to E and I). But, these can also mix together to from hybrids, and we know of at least 89 hybrid subtypes (I won’t list the names for all of those).
Things get a bit controversial with subtypes because HIV-1 M subtype B is the most common in the UK and the rest of Western Europe, as well as the Americas and Australia. This also means it’s the one we have done the most research on. But, subtype B represents about 12% of HIV cases, while 50% of people living with HIV worldwide have subtype C (mainly in Africa and India), and there’s much less research on this type of HIV.
Once again, thanks to AVERT and check out their awesome page for more info about the different types of HIV.
So what about this new HIV?
The recent study looked at a variant within HIV-1 M subtype B representing comparatively small changes to the virus. It was created sometime around the year 2000 and the study found about 100 people in the Netherlands living with it. It’s part of an ongoing research study called BEEHIVE that is monitoring people living with HIV.
The research compared the variant, which they call VB, against other people living with HIV. People with the VB variant had a viral load that could be more than five times higher, suggesting a much greater risk of transmission. The infection also progressed faster. For males in their 30s, on average, HIV progesses to the advanced stages in about three years from diagnosis if left untreated. The study estimated that the VB variant typically took just nine months.
These sound like big changes, but the variant can still be treated with all the usual drugs, so people living with HIV can still be treated and we can still prevent the spread of this variant just as easily by using protection and by taking PrEP. But this research helps to highlight that HIV can change and can become more harmful, which shows us why taking precautions is important and why taking care of our sexual health and helping to end the HIV epidemic now could help us all to avoid more harmful types of HIV in the future.
If you’re HIV-negative and you have sex, find out more about PrEP for HIV prevention, and ask for personalised advice at your sexual health clinic. Our free Preptrack app can help you to stay on top of PrEP, giving you confidence in your HIV protection so you can have sex without the stress.